Breast Reconstruction & Body Contouring
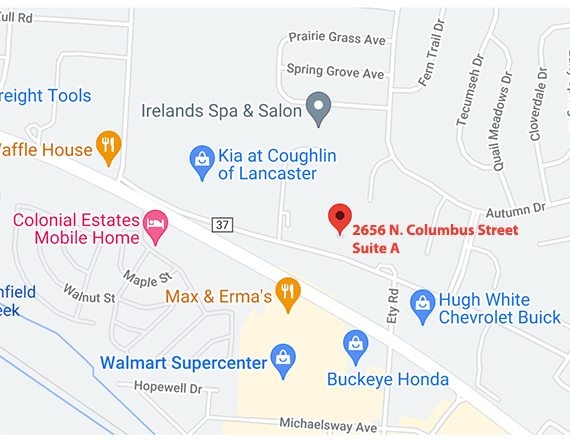
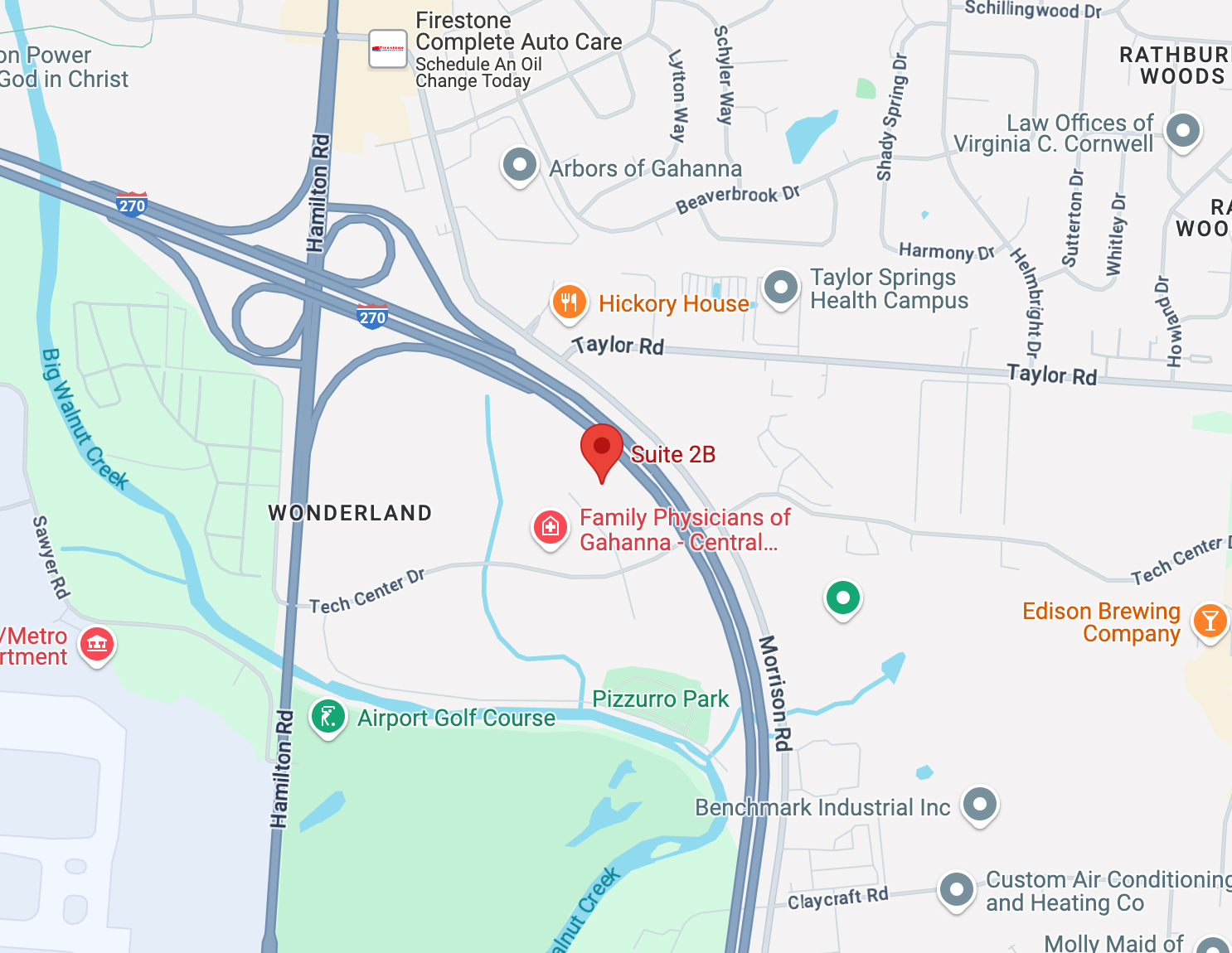
Conveniently located to serve Columbus, Lancaster, Pickerington, and Canal Winchester
Jump To
For women who have undergone mastectomy (removal of the breast due to cancer or a pre-cancerous condition) or women who have a breast deformity, breast reconstruction offers the means to restore their womanly shape and, in turn, to restore their self-confidence.
“My goals were for my breasts to look natural but the results were better than I expected. The doctor made me feel like I was talking to a friend and everybody in the office too.”
Breast reconstruction is a very delicate procedure in which both timing and technique are important. Surgery may be performed immediately following a mastectomy or at a later time. Reconstruction may be done with a tissue expander and implant, or through utilizing your body’s own tissues (flap reconstruction). The combination of options that is best for you is something you should determine in conjunction with your breast surgeon, oncologist, and with Dr. Lichten.
“Dr. Lichten did a remarkable job in finishing my breast cancer reconstruction. He built nipples out of nothing and reshaped them to look completely natural. He fixed the damage done by other surgeons. I only regret not finding him first! He made the memory of my cancer disappear being the gifted surgeon he is.”
After the initial reconstruction, patients may undergo further operations to exchange the tissue expander for a permanent implant, revise the reconstructed breast, reconstruct the nipple and areola, or perform an operation on the opposite breast to achieve better symmetry. Dr. Lichten and everyone at Central Ohio Plastic Surgery will help you through every step of the reconstruction process.

Patients often worry about insurance coverage for breast reconstruction after mastectomy. In 1998, Congress passed the Women’s Health Act which mandated insurance coverage for all phases of breast reconstruction related to breast cancer. You can get more information from the Department of Labor Website here.
Click here to read an article on breast reconstruction options after mastectomy by Dr. Lichten.
Breast Cancer Reconstruction Q&A
Dr. Lichten participated in a Q&A for Komen Columbus about breast cancer reconstruction. You can view his full interview here or below:
+ What is the approximate “life expectancy” of silicone breast implants? When, if ever, to they need to be replaced and how do you know (signs/symptoms) when replacement is warranted?
Silicone breast implants are one of the most studied medical devices in history. According to manufacturer research, the rupture rate for the most commonly used silicone implants is about 10% after 17 years. In addition, there are other issues that could arise at the surgical site, even if the implant remains intact. For example, a woman may develop capsular contracture, which happens when the scar capsule around the implant hardens; or fluid may develop around the implant site. I recommend that my patients see me once a year in follow up, or more often if there is a change, so that I can examine the implants and the surgical site. The FDA also recommends that patients get an MRI after 5-6 years and every 2-3 years after that to check the implants for rupture.
+ I’ve completed my breast cancer therapy which consisted of a mastectomy, chemotherapy and radiation. What is the best reconstruction for me?
The only person who can ultimately decide what reconstruction option is right for you, is you. There are various techniques, which give women more choices to restore their shape after mastectomy. The main reconstructive options involve either using a tissue expander/implant or using your own tissue, muscle and skin from another part of your body to rebuild the breast using a flap technique. The most common flaps use a portion of a patient’s abdominal muscle, tissue and skin (the Transverse Rectus Abdominus Muscle or TRAM flap), or using the muscle from the back (Latissimus Dorsi Flap) along with an implant for volume to recreate the appearance of a breast. Other techniques involve removing tissue completely and then re-establishing a new blood supply (free flap reconstruction). Each surgery has its own risks and benefits, so discuss how these relate to you with a board certified plastic surgeon.
Each option can be performed either during the mastectomy surgery as an “immediate” reconstruction, where the process is started at the time of the mastectomy, or later as a “delayed” reconstruction months to years after having a mastectomy. The right choice varies for each woman, depending upon your lifestyle, treatment plan, body type, general health, and your goals. You will work with your plastic surgeon to determine the best individualized plan.
There is one specific aspect of your history that it is worthwhile to discuss here – specifically if you have had radiation to the chest wall following your mastectomy. Radiated skin makes tissue expansion much more difficult and adds additional risks to wound healing after surgery. Most plastic surgeons would opt for and recommend to their patients a flap technique as described above for better chances at success for breast reconstruction after mastectomy in the face of previous radiation.
+ Is it ever too late to reconsider reconstruction after cancer treatment is finished?
No. It is never too late to consider reconstruction. I have performed a breast reconstruction more than ten years after my patient’s mastectomy. The reconstruction process is very personal and it is important that the timing and pace works for you.
This is important information, because nationwide, a staggering 5 out of 10 mastectomy patients are not told that they have the option of reconstruction. For these women, delayed reconstruction may be an option to close the loop on a process that started years earlier.
+ What kind of questions should I be sure to ask about my treatment to make sure I have the best chance at a successful reconstruction?
The most important questions to ask are designed to make sure you are comfortable with the doctor performing your treatment. You want to make sure that your doctor is Board Certified in Plastic Surgery. This will assure you that s/he has had the right background and training to handle your specific treatment. You will also want to know how many times s/he has performed the type surgery that you are planning and how much experience s/he has with breast cancer reconstruction.
In terms of a game plan for treatment, you and your surgeon should discuss the different options for treatment (see the question above) and the timing of the surgeries (whether you should have immediate or delayed reconstruction). This will help you to create a personalized treatment plan that best suits your health, lifestyle and goals.
+ I’ve heard a lot about fat injections lately. Is that an option to help with reconstruction results?
Yes. Fat transfer is a common part of secondary breast surgery. After permanent implants have been placed or a TRAM flap has been performed, fat transfer can smooth out irregularities or soften transitions from implants to the native chest. Most commonly, I will use belly fat for this procedure. Since this is a part of breast reconstruction, it should also be covered by health insurance.
+ Are silicone implants safe?
In 1992, the FDA took silicone breast implants off the market for cosmetic use. They remained available for women who needed breast cancer reconstruction during that time. In 2006, the FDA determined that silicone implants were safe and allowed them back on the market for general use for women over age of 22. The vast majority of studies and research done on silicone during that time confirm that silicone implants pose no additional risk over saline implants.
In August 2019, the FDA stated: “to protect individuals from the increased risk of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL), associated with Allergan BIOCELL textured breast implants, the Food and Drug Administration (FDA) requested that Allergan recall its BIOCELL textured breast implants and tissue expanders. Allergan agreed and is removing these products from the global market.”
BIA-ALCL is a very rare lymphoma of the capsule that forms around a breast implant. To date, all cases have been associated with textured implants (which represents less than 5% of the implants we typically use at Central Ohio Plastic Surgery), at a rate of less than 1 in 3,000 cases. It usually presents 8 to 10 years or more after implant placement as a fluid collection (swelling) around the breast implant. Removal of the implant and capsule is curative.
If the safety and of silicone implants is a concern, we invite you to do research of your own. It is our opinion, however, based on research and education, that medically and scientifically, silicone breast implants pose no significant additional risk.
+ What are my options if I’m not satisfied with the results of my reconstruction?
If you have concerns about your surgical results, without question, the first thing you should do is go back and talk to your surgeon. Have an open and honest conversation about what bothers you and the two of you should be able to develop a plan to help meet your expectations.
Perhaps the most important way to help you be satisfied is to have a conversation with your plastic surgeon before your surgery to create realistic expectations of what surgery and reconstruction can do for you. The goal of most reconstructions is to make the patient appear and feel normal in clothes and a bathing suit. Reconstruction surgery is not the same as a breast augmentation, and the results will not look the same. In addition, you will not have the same sensation that you used to, and you will likely have scars on your breasts. Having said that, however, there are many options and results are better than they have ever been.
+ How should I expect my reconstruction appearance to change over time?
As a general matter, the appearance of implants should not change all that much. There can be changes related to the capsule around the implants, but for the most part, implants should remain stable. That said, as you age and gain or lose weight, it is possible the implants may appear bigger or smaller than they used to look as the proportions of your body change in relation to the implants.
A flap reconstruction may sag or droop just as your native breast may over time. It will respond to weight changes as your body does, but this can be variable, again leading to potential changes in the relative appearance of the breast.
In addition, if you have to undergo radiation or chemotherapy after your reconstruction, those treatments may cause the reconstructed area to shrink or tighten over time. Therefore, if you know in advance that radiation or chemotherapy may be part of your treatment regimen, it is critical that you advise your plastic surgeon, so you can coordinate those therapies for the best result.
+ How do I know if my doctor is qualified to perform my surgery?
No one can guarantee your results. You can, however, ensure that your doctor has had the right training, by confirming that s/he is board certified by the American Board of Plastic Surgery. Although many physicians claim to be board certified, you should confirm their specialty. In addition, you can gain comfort if your doctor is a member of the American Society of Plastic Surgeons (ASPS). The ASPS confirms plastic surgeons’ background training and education. In addition, they ensure that the doctor keeps up on the latest medical developments and research.
Articles
Contact us at 740-653-5064 or 614-862-8008 or request a consultation online today.